At a press briefing April 14, state Secretary of Health John Wiesman told Washingtonians to prepare for living in a “new normal” of social distancing “for many, many months” to continue slowing the spread of the novel coronavirus that causes COVID-19.
Wiesman said the disease won’t be stopped until treatments and a vaccine are developed, which are still a year away. More than 140 experimental drugs and vaccines are being developed around the world, he said.
Until then, people will likely need to continue social distancing and he recommended wearing masks in public, though he said there could be “partial easing” of the current restrictions that were put in place to prevent hospitals from being overwhelmed.
Wiesman made his announcement the same day President Donald Trump said the federal government was preparing guidelines for the states to reopen closed businesses and return people to work, adding that he had “absolute authority” to compel state governments to obey.
Trump later said he would be “authorizing” states to reopen as soon as May 1, before the federal recommendation on closures and distancing end. He eventually offered a three-step plan that states could follow, saying governors would be the ones to decide and “would be held accountable.”
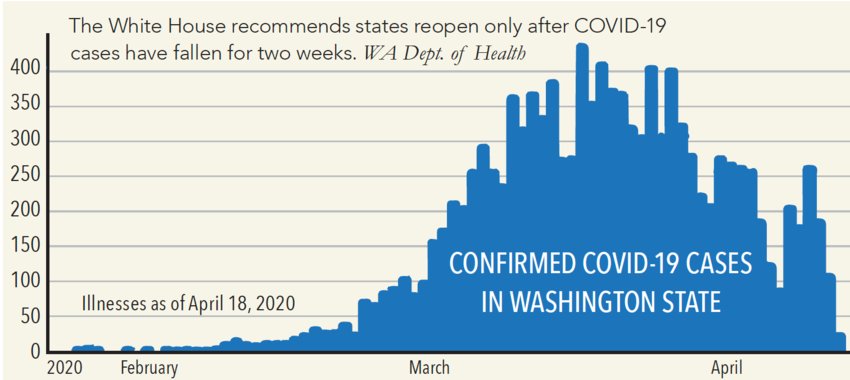
Gov. Jay Inslee and the DOH have been more cautious, concerned that lifting restrictions prematurely could trigger a resurgence of infections, exacerbating damage to the economy that may exceed the Great Depression. Inslee has already closed schools and the stay-at-home order and partial business closures should end May 4, but he has also said the order may be extended. “We will make decisions at that time based on the data and science, and how much progress we’re making,” Inslee said April 10.
The U.S. lagged behind other countries testing its population for COVID-19, initially refusing to use tests from the World Health Organization and then issuing faulty tests from the U.S. Centers for Disease Control and Prevention. By April 18, the U.S. was testing 150,000 people a day, about the same as South Korea, which saw a decline in infections and began to lift some of its restrictions.
“We will make decisions at that time based on the data and science."
However, South Korea tested on a much larger scale than the U.S. — finding one confirmed COVID-19 case for every 52.4 people tested — producing a more comprehensive picture of the virus spread and retreat than the U.S. has so far achieved, having found one case for every 5.3 tests.
“Anyone can get tested,” according to the DOH website. “However, healthcare providers are focusing on people with symptoms of COVID-19. While testing supplies are still limited, they are also prioritizing certain groups of people at this time.”
The result has been that only the sickest people get tested while the remainder recover at home, perhaps never reporting their symptoms, which could lead to a drastic under-counting of cases and cause a slowdown in delivery of resources for medical personnel, according to the CDC.
Washington state is also conducting a random serum survey with the CDC to determine who may have antibodies to COVID-19, according to Dr. Kathy Lofy, the state health officer and chief science officer.
“It gives us information on how many people may be immune in Washington,” she said. “Once we know that information, that will help us better understand how many people have been infected and help us understand how much longer we have to go to continue these social distancing measures.”
But it is not known at this time whether antibodies result in meaningful immunity that can lead to herd immunity, where enough people have been exposed and recovered to protect those who haven’t. Herd immunity is usually achieved through vaccination rather than exposure.
In mid-March, the United Kingdom was still open for business and encouraging only the sick and vulnerable to self-isolate. Social distancing and closures came only after a study by the Imperial College indicated there might be as many as 250,000 deaths in the UK before herd immunity was achieved.
By mid-April, the COVID-19 death rate in the UK was 12.7 percent; in the U.S. it was 4.1 percent. The global rate was 6 percent.
According to a recent report in Scientific American, immunity functions on a continuum. People who get chicken pox almost always develop long-lasting resistance. In contrast, people with HIV often have large amounts of antibodies that do nothing to prevent or clear the disease.
Immunity to seasonal coronaviruses that cause the common cold start to wear off about two weeks after someone is sick. They can get the same cold again within a year.
The novel coronavirus resembles those that caused SARS (severe acute respiratory syndrome) in 2002 and MERS (Middle East respiratory syndrome) in 2012. Studies of SARS showed that immunity peaks at around four months and offers protection for two or three years after infection. There have been no known cases since 2004. Though widespread at the time, researchers believe it was unable to gain a lasting foothold in the population because it was quickly contained.
A CDC study of MERS survivors found that their antibodies lasted about six months after infection. Individual cases and outbreak clusters continue. With a mortality rate of nearly 40 percent, it is closely monitored. There is no vaccination or treatment for SARS or MERS.
UNDERWRITTEN BY THE FUND FOR NONPROFIT NEWS (NEWSMATCH) AT THE MIAMI FOUNDATION, THE ANGEL GUILD, ADVERTISERS, DONORS AND PEOPLE WHO SUPPORT INDEPENDENT, NONPROFIT LOCAL NEWS