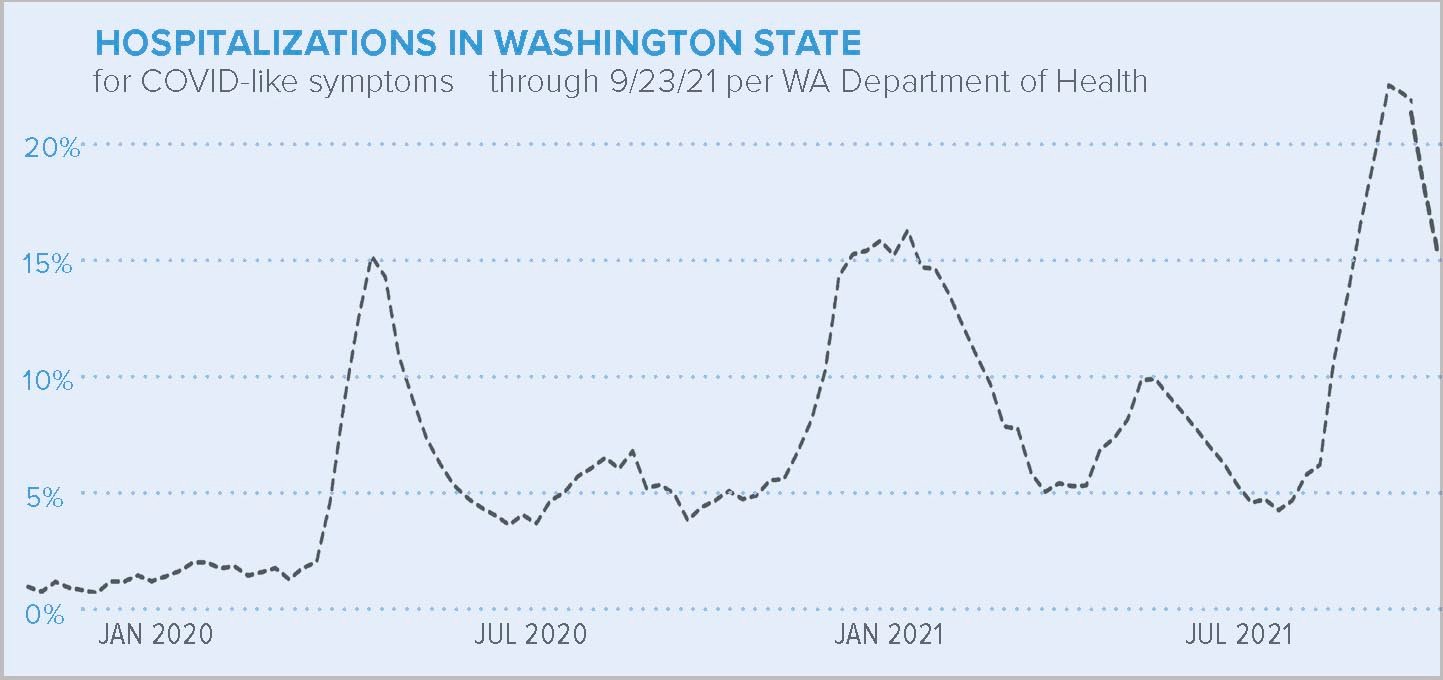
Hospitals across the state are at or near capacity as the highly contagious delta variant of COVID-19 spreads among the population, according to the Washington State Department of Health.
St. Anthony Hospital in Gig Harbor is no exception. From Aug. 6 to Sept. 3, all 218 beds were occupied, along with 14 of its 16 intensive care unit beds.
At the beginning of the month, the seven-day average of COVID-19 patients admitted was 26. There were 153 confirmed COVID-19 emergency room visits out of 920 between Aug. 28 and Sept. 3. Across the Virginia Mason Franciscan Health System, which includes St. Anthony, there are over 200 COVID-related hospitalizations and 28 COVID-positive patients in ICUs, according to the St. Anthony communication department.
“Hospital capacity is currently stressed across the state of Washington,” the DOH said in a Sept. 8 statement, warning that the growing strain on the medical system could force hospitals to postpone urgent and elective procedures to preserve resources for patients with life-threatening conditions.
This means, like during the worst spikes of cases in 2020, patients scheduled for surgeries requiring multiple-day post-procedure observation and care may have to wait for the current wave of COVID-19 cases to recede before they can get into the operating room.
By mid-September, Oregon and Idaho declared crisis standards of care in many of their medical facilities. The declaration allowed hospitals to make significant changes to rationing health care, like allocating ICU rooms to patients who are more likely to survive. This means a ventilator is more likely to go to someone who is otherwise healthy and will recover than someone who doesn’t have as good a chance.
Idaho hospitals are seeking relief from the increased number of COVID-19 patients by requesting transfers for those patients to facilities in Washington, most of which are already at a deficit for staff themselves. CHI Franciscan Health is, in some cases, offering incentive pay to ensure their facilities are appropriately staffed, it said.
The DOH asked the U.S. Department of Health and Human Services Sept. 22 for more federal medical personnel to staff hospitals and long-term care facilities statewide in addition to what has already been provided.
“We know that COVID-19 patients, those seeking care for other medical reasons, along with staff shortages, have all put stress on our current hospital system,” said state Secretary of Health Umair A. Shah, MD, MPH.
DOH has also asked health care practitioners and retired medical professionals to volunteer to support hospitals vaccination efforts during the latest COVID-19 surge.
Most hospitalized patients are unvaccinated and of those who are vaccinated, many have co-morbidities that have weakened their immune system, according to the Centers for Disease Control and Prevention.
A Sept. 10 report from the CDC showed Washington’s weekly infection rate of new COVID-19 cases was 300 per 100,000 people with a total active case count of 22,876, or about 1 in 333 residents. Admissions for new confirmed COVID-19 cases into hospitals was 9.5 out of every 100 beds. Deaths from COVID-19 were at 2.7 per 100,000 cases.
Sixty-eight percent of Washington’s population has been fully vaccinated while Idaho’s vaccination rate is around 41% and Oregon is at 59%. Nationwide it’s 55%.
The Key Peninsula has the lowest vaccination rate compared to Pierce and neighboring counties, averaging 41%. Pierce has a 64% rate; Kitsap is at 65% and Mason at 58%.
The U.S. currently has 17% of new COVID-19 infections around the globe despite having the best vaccine supply, according to the CDC. The increase is especially obvious among children, who make up 20% of the nation’s new cases, apparently becoming infected by unvaccinated adults in the home.
More than 177 million Americans are vaccinated against COVID-19, but cases have spiked nationally to 140,000 per day, including 1,000 deaths per day, according to the CDC. Most of the severe illness and death is occurring among the unvaccinated. Breakthrough infections in vaccinated people also occur but are less dangerous.
While the delta variant has increased hospitalizations, after re-introducing the indoor mask mandate Aug. 23, COVID-19 cases in the state plateaued compared to July numbers. However, with infections that occurred over the Labor Day weekend still pending and the Washington State Fair currently in progress, transmission among large crowds is a major concern for health care workers. There is already a Tacoma-Pierce County Health Department contact tracing investigation underway involving 20 fair workers and attendees who were at the fair during their contagious or exposure period.
The infection rate on the Key Peninsula averaged 1 per day from Feb. 1 to July 30, according to TPCHD. It increased to 12 per day by Sept. 9.
That spike followed a summer of more open behavior denied to the KP since 2019, including an all-peninsula-church gathering at Gateway Park July 25, a Peninsula High School reunion at the KP Civic Center Aug. 14 and other public events.
Total cases on the KP stood at 914, including seven deaths, at press time.
UNDERWRITTEN BY THE FUND FOR NONPROFIT NEWS (NEWSMATCH) AT THE MIAMI FOUNDATION, THE ANGEL GUILD, ADVERTISERS, DONORS AND PEOPLE WHO SUPPORT INDEPENDENT, NONPROFIT LOCAL NEWS